AbstractBackground and ObjectiveSleep deprivation is a significant issue among adults. It is on the rise in contemporary society, largely influenced by the shift towards a 24/7 lifestyle and long working hours. Lack of sufficient sleep can influence immune function causing systemic inflammation. Inflammation is a shared characteristic between chronic periodontitis and sleep deprivation. In addition, sleep deprivation can have detrimental effects on cognitive function and motor skills, which may reduce the individual’s ability to maintain proper oral hygiene further influencing periodontal health. This study aimed to examine the quality and duration of sleep and their potential association with periodontitis in the South Indian population.
MethodsFifty-six subjects were diagnosed based on the criteria outlined in the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. Probing depth and clinical attachment loss were measured as a part of the clinical examination. The severity, complexity, and progression of periodontitis were classified based on both stage (I–IV) and grade (A–C) systems. The participants were given a questionnaire including demographic information and the Pittsburgh Sleep Quality Index.
ResultsThere was a significant association between the severity and extent of periodontitis and sleep quality and duration. The mean sleep quality was highest in Stage IV (1.57 ± 0.76) and Grade B (1.62 ± 1.28). Similarly, Stage IV (1.14 ± 0.66) and Grade B (1.38 ± 0.92) showed the highest scores for sleep duration.
INTRODUCTIONPeriodontitis is a chronic inflammatory disease caused by microbes that persist in susceptible individuals. It is due to mutually reinforcing interactions between the dysbiotic microbiome and the host inflammatory response [1]. Periodontal diseases are not limited to oral tissues, as bacteria and inflammatory mediators associated with these diseases can enter the bloodstream and have systemic effects, contributing to inflammation throughout the body. Multiple factors can increase an individual’s susceptibility to periodontal diseases and influence the progression and severity of the condition [2]. They include gender [3], smoking [4] and alcohol (lifestyle) [2], diabetes [5], obesity [6], metabolic syndrome [7], stress [8], and genetic factors [9].
Based on data derived from the Global Burden of Diseases Study conducted in 2017, there were 796 million reported cases of severe periodontitis worldwide. Furthermore, from 1990 to 2019, the global prevalence of periodontitis increased by 99.0% [10]. A recent systematic review and meta-analysis examining the prevalence of periodontal diseases among adults in India revealed that approximately 51.0% of the population had periodontal diseases. This indicates that nearly half of the Indian adults, equivalent to approximately 320 million individuals, are affected by some form of periodontal disease [11].
About one-third of our lives, on average, is spent asleep [12]. In the last decade, there has been a significant increase in research focused on the relationship between sleep and health. Sleep is a naturally occurring process mediated by the central nervous system, which plays a dynamic role in regulating the immune system. Sleep deprivation can alter physiological systems that impact the distribution of immune cells and the production of inflammatory cytokines. When sleep is disturbed, changes occur in the systems that regulate the immune response, leading to an abnormal increase in inflammatory responses [13]. From a biological perspective, there are plausible mechanisms that establish a connection between inflammation and sleep deprivation in both causal directions. During sleep deprivation, the activation of the autonomic nervous system and increased levels of catecholamines can stimulate the production of inflammatory mediators. Additionally, sleep deprivation can lead to elevated blood pressure, which may increase endothelial shear stress. This, in turn, triggers the production of inflammatory mediators like interleukin 6 (IL-6) and adhesion molecules such as e-selectin and soluble intercellular adhesion molecule-1 by the endothelial cells [14]. Furthermore, prolonged activation of the hypothalamic-pituitary-adrenal axis following sleep deprivation has notable impacts on hormonal profiles and could potentially play a role in the onset of cognitive impairment [15].
According to observations, over 50% of the Indian population is suffering from sleep deprivation. Approximately 26% of the population sleeps for less than 8 hours per day. This trend may be attributed to the changing socioeconomic and cultural profile of Indian society [16]. Sleep can potentially influence periodontal disease as sleep deprivation can contribute to increased systemic inflammation, which can further enhance periodontitis. Hence present study intended to assess the quality and duration of sleep and their possible association with periodontitis in the South Indian population.
METHODSStudy Design and PopulationThe current study comprised periodontitis patients who reported at the Department of Periodontology, in a private dental school in Mangalore from July 2022 to January 2023. The subjects in the current study included patients aged between 30 and 59 years. Patients who had a minimum complement of 20 natural teeth and a history of smoking or using smokeless tobacco products, patients who consume alcohol, patients on any medication or with any systemic diseases, pregnant and lactating women, who had undergone periodontal therapy in the past 6 months, and any subjects with an incomplete questionnaire were excluded from the study.
Ethical StatementInformed consent forms were signed by all the participants prior to the commencement of the study. The study mandated that the participants read, comprehend, and sign an informed consent form, and they had to be willing and capable of complying with the study requirements. The institutional ethics committee reviewed and sanctioned the study protocol under protocol number ETHICS/ABSMIDS/269/2022. The privacy and confidentiality of the participants were carefully upheld during both the study and analysis periods.
Sample Size CalculationOverall, based on the 5% level of significance, standard deviation of the Pittsburgh Sleep Quality Index (PSQI) score in periodontitis is 1.33, the estimated error is 0.35, and the total sample required is 56. This is calculated using nMaster software version 2.0 (Department of Biostatistics, Christian Medical College, Vellore, India) [17].
Data CollectionThe study involved two main components: a clinical examination to diagnose periodontitis and a questionnaire. The questionnaire included demographic information such as age, sex, and the PSQI. The periodontal examination was conducted prior to the completion of the PSQI questionnaire, reducing the potential impact of examiner bias.
The clinical examination involved measuring periodontal pocket depth (PD) and clinical attachment loss (CAL). These were assessed at six sites per tooth. Two calibrated examiners used William’s periodontal graduated probe (Williams Colorvue TM Probe, Hu-Friedy ® ; Chicago, IL, USA) to conduct the clinical examination. To measure the PD, a periodontal probe was carefully inserted into the pocket, following the vertical axis of the tooth until it reached its deepest point. The distance between the base of the pocket and the gingival margin was then recorded with precision to the nearest millimeter. Similarly, CAL was determined by measuring the distance between two specific reference points, the cementoenamel junction, and the base of the pocket.
Participants were determined as having periodontitis if they exhibited interdental CAL in at least two nonadjacent teeth, or if they had buccal or oral CAL of 3 mm or more with a PD of 3 mm or more in at least two teeth. The classification of periodontitis was determined using a system based on both the staging and grading of the condition. The severity, complexity, and progression of periodontitis were classified based on both stage (I–IV) and grade (A–C) systems. Stage determined the severity and complexity of the condition, while grade estimated the likelihood of disease progression. If certain complexity factors were present, the stage could be elevated to a higher level, and if specific risk factors were present, the grade could also be elevated to a higher level [18].
All participants in the study were provided with a PSQI questionnaire. PSQI was designed to provide a dependable, valid, and standardized measure of sleep quality, to differentiate between good and poor sleepers over one month. The assessment focuses on evaluating the quality and patterns of sleep using a questionnaire that contains 19 self-rated items. In this study, these items were categorized into 7 domains to examine various aspects of sleep. All participants provided ratings for each of the seven dimensions of sleep. A cumulative score of “5” or above indicated subpar sleep quality, with higher PSQI scores representing deteriorating sleep quality [19].
Statistical AnalysisDescriptive analysis was conducted and presented as mean and standard deviation. Data was checked for normality before being subjected to analysis; the Shapiro-Wilk test was done. Data was analyzed using IBM SPSS (version 26, IBM Corp., Armonk, NY, USA). One-way ANOVA was used to find the significance between stages and grades, and the threshold for statistical significance was established at a level of 0.05.
RESULTSFifty-six subjects (28 females and 28 males) were enrolled in this study based on the guidelines provided by the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions [18]. The mean age of the subjects was 41.80 ± 5.80 years, ranging from 30 to 59 years. Stage IV and Grade C had the highest mean age (Table 1). Since age is a significant confounding variable, we subdivided the age group into two categories, 30–45 years and 46–60 years, to reduce its impact on the study. The findings indicated a notable association between age and sleep quality, but age did not demonstrate any association with sleep duration (Supplementary Table 1 in the online-only Data Supplement).
In the present study, the mean CAL was 4.34 ± 2.49 mm and PD was 4.18 ± 1.89 mm. The mean PD and CAL were highest in Stage IV and Grade C subjects (Table 2).
The PSQI consists of 7 domains (Table 3), among these, the mean sleep quality score was highest in Stage IV (1.57 ± 0.76) and Grade B (1.62 ± 1.28) subjects, followed by Stages III, II, and I subjects and Grades C and A subjects, respectively (Fig. 1). Tukey’s post-hoc analysis was further done and it revealed a statistically significant association between stages I and III and between stages I and IV in terms of sleep quality.
Stage IV (1.14 ± 0.66) and Grade B (1.38 ± 0.92) showed the highest scores for sleep duration (Fig. 2). Post-hoc analysis results showed a statistically significant association between sleep duration and stages I and III, and between stages I and IV. These results suggest that there is a significant association between the severity and extent of periodontitis and both sleep quality and sleep duration.
The highest score among the 7 domains was for daytime dysfunction which was seen in Stage IV (2.43 ± 1.09) and Grade C (1.88 ± 1.22) periodontitis patients, which may have resulted from poor sleep quality and lesser duration of sleep. Meanwhile, the lowest score among the domains was seen in sleep efficiency in Stage III (0.60 ± 0.83) and Grade B (0.52 ± 0.81). Component 6, which consisted of the use of sleep medication was negligible as none of the subjects used any form of sleep medication.
The mean global PSQI value was highest in Stage IV (8.36 ± 2.13) and Grade B (7.33 ± 3.69), followed by Stages III, II, and I and Grades C and A, respectively. A total score of “5” or more indicated poor sleep quality and higher PSQI scores corresponded to worse sleep quality.
DISCUSSIONPeriodontal disease is characterized by intricate and dynamic interactions involving specific bacterial pathogens, detrimental host immune responses, and environmental factors. These components interact in a complex manner to contribute to the development and progression of periodontal disease [20]. The host immune response to periodontitis leads to the production of various inflammatory mediators such as cytokines, eicosanoids, kinins, complement activation products, and matrix metalloproteinases [21]. These mediators further promote the inflammatory response and contribute to the destruction of connective tissue and bone. The process of bone resorption in periodontal disease is influenced by the release of inflammatory cytokines such as IL-1, IL-6, IL-11, IL-17, and tumour necrosis factor-alpha (TNF-α), along with other factors like leukemia inhibitory factor and oncostatin M [22].
A systematic review conducted in 2016 by Irwin et al. [23] validated the correlation between sleep disruption and three indicators of systemic inflammation, C-reactive protein, IL-6, and TNF-α. Both inadequate and excessive amounts of sleep have been linked to decreased overall health. During sleep deprivation, the autonomic nervous system is activated and there is an increase in the level of neurotransmitters and hormones, which can stimulate the synthesis of inflammatory mediators [24]. Sleep disorders are often associated with elevated levels of inflammatory cytokines, such as IL-1β, IL-6, and TNF-α, which are markers of inflammation [25]. Therefore, sleep deprivation leads to a decrease in immune function and triggers systemic inflammation. As inflammation is a common feature of both chronic periodontitis and sleep deprivation, the role of cytokines in the development of chronic periodontal disease in sleep-deprived individuals may lead to an exacerbation of periodontal destruction through a potential synergistic effect.
Conversely, cytokines can directly impact the brain, particularly areas involved in regulating sleep. It plays a crucial role in the body’s defense against infections, and increased levels of cytokines, such as IL-6, can induce sleep. This may explain why during infections or inflammatory diseases, individuals may experience longer sleep durations as part of the body’s immune response [14]. These mechanisms suggest a bidirectional relationship between sleep and inflammation, where sleep disturbances can lead to increased inflammation, and inflammation can disrupt normal sleep patterns.
While the literature has explored the connection between periodontal disease and sleep, no research currently examines the association between stage and grade of periodontitis on sleep quality and sleep duration in the South Indian population. In the present study, PSQI was used to determine the sleep quality and sleep duration. The PSQI is a well-known instrument used to measure sleep quality and disturbances over 1 month. Its main objective is to offer a comprehensive assessment of an individual’s sleep patterns and overall sleep quality across multiple domains, including sleep duration, sleep efficiency, sleep latency, sleep disturbances, use of sleep medication, and daytime dysfunction. The PSQI generates a single score that spans from 0 to 21, where higher scores signify lower sleep quality. It also offers a straightforward index for patients to complete and for clinicians and researchers to interpret [19]. Moreover, the PSQI exhibits a sensitivity of 75.0% and a specificity of 88.9% in accurately differentiating between individuals with good and poor sleep when using a global score cut-off of 6 in the Indian population. Additionally, it exhibits good internal consistency and reliability, with a Cronbach’s alpha coefficient of 0.736 [26]. Numerous studies have consistently supported the high validity and reliability of the PSQI [27,28]. While the PSQI is valuable in assessing sleep quality, it is not intended to diagnose specific sleep disorders. If the results of the PSQI suggest the presence of a sleep disorder, it is advisable to seek further assessment by a healthcare professional, such as a sleep specialist, for proper diagnosis and management.
The results of the current investigation indicated a significant statistical association between sleep quality and duration, and periodontitis. These results were in accordance with the findings of Grover et al. [17] where the periodontitis group had the highest mean PSQI score compared to the healthy and gingivitis groups, indicating a greater level of sleep disturbance in individuals with periodontitis. These results were further supported by an animal study in rats where fatigue due to deep sleep deprivation for 7 days was found to have a detrimental effect on systemic health, worsening gingival inflammation, and alveolar bone loss in experimentally induced periodontitis.
The findings of this study align with various nationally conducted surveys, indicating a substantial correlation between sleep quality and sleep duration, and periodontitis [29-33]. According to a study [29], individuals who maintain a regular sleep duration of over 7 hours per night without experiencing difficulties falling or staying asleep have a 40% lower likelihood of developing severe periodontal disease. On the other hand, in a different study [31], it was observed that individuals who experienced insufficient sleep had a 19% increased likelihood of developing periodontitis compared to those who had adequate sleep. This suggests that an adequate amount of sleep and good sleep quality may play a protective role in maintaining oral health and reducing the severity of periodontal disease.
Meanwhile, a study in the Korean population [30] on sleep duration and time showed contradictory results as they suggested that both an unusually extended period of sleep duration and a preference for daytime sleeping are linked to a higher risk of developing periodontitis. These conflicting results could be influenced by several confounding factors that were not adequately controlled in the research design. Among them, other health problems or underlying conditions in individuals with longer sleep duration could also contribute to the observed results. To overcome this, in this study, we tried to minimize patient-centered confounders, strict exclusion criteria were implemented, excluding individuals who were engaged in smoking both past and present, pregnant, or lactating, had preexisting systemic conditions, underwent recent periodontal treatment within the last 6 months, or had a history of medication use (including antibiotics or anti-inflammatory drugs) within the past 3 months. These measures aimed to provide a study sample with minimal patient-centered confounders and enhance the reliability of the findings.
In a cross-sectional study conducted on the Korean population in 2017 [32], a unique and independent connection between extended sleep duration and the occurrence of periodontitis was discovered. The authors of the study suggested the possibility of a “reverse causation” effect, implying that periodontitis could potentially impact sleep duration, or that there might be a bidirectional relationship between the two factors.
In the current study, there was also a statistically significant relationship between the stage and grade of periodontitis and the scores of the 7 domains in the PSQI. The mean sleep duration and quality were the highest in Stage IV periodontitis subjects, while Grade B periodontitis subjects showed greater association which partially agrees with the results obtained by Karaaslan et al. [34]. The post-hoc analysis did not show any significant association between the sleep duration and quality of Grade B and Grade C subjects. These contradictory results may be due to the unequal distribution of the subjects across different stages and grades.
LimitationsWhile this study has several positive aspects, it is crucial to acknowledge and address its limitations to ensure a comprehensive understanding of the research findings. First, sleep duration and quality were self-reported by the subjects. The self-reporting by the participants introduces the possibility of subject bias in the study. Since the sleep duration is based on an individual’s perception and memory, there may be variations and inaccuracies in their reporting. Factors such as recall bias or subjective interpretations of sleep duration could affect the accuracy of the data collected. Second, the study is designed as an observational, cross-sectional study; hence, longitudinal studies are recommended to validate the findings of the current analysis and to investigate potential causal relationships. Third, although we made efforts to adjust for several potential confounding variables in our analyses, factors such as socioeconomic status, lifestyle behaviors, and genetic predispositions could also play a role in the relationship between sleep and periodontitis. Oral hygiene practices are an important confounding factor of both sleep disturbances and periodontitis, and not being able to asses this due to either self-reported bias, inability to utilize objective measures, and study design is one of the drawbacks of this study. These unmeasured variables may introduce confounding effects that were not accounted for in our study. Further research with a larger sample size, comprehensive measures, and adjustments for a broader range of confounding factors and a longitudinal design is needed to provide a more thorough understanding of the relationship between sleep and periodontal disease.
ConclusionThe findings of this study suggest a significant association between periodontal diseases, and inadequate sleep quality and duration in the South Indian population. In addition, insufficient sleep has negative impacts on immune function, cognitive function, and motor skills, potentially hindering a person’s ability to maintain proper oral hygiene. Consequently, it increases the likelihood of developing periodontal disease. Hence, poor sleep quality and insufficient sleep duration may potentially be considered risk factors for the development of periodontitis. However, it is important to note that the present investigation has its limitations, and further research is needed to establish a more definitive and causal relationship between sleep and periodontal diseases.
Supplementary MaterialsThe online-only Data Supplement is available with this article at https://doi.org/10.17241/smr.2023.01767.
Supplementary Table 1.Association between age and sleep quality and duration NOTESAvailability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Author Contributions
Conceptualization: Gauri Jayachandran, Biju Thomas. Data curation: Gauri Jayachandran, Karthika Ganesh. Formal analysis: Sruthi Vijayan, Smitha Shetty, Mamatha Shetty, Amitha Ramesh. Investigation: Gauri Jayachandran, Karthika Ganesh. Methodology: Gauri Jayachandran, Biju Thomas, Sruthi Vijayan. Project administration: Gauri Jayachandran, Biju Thomas, Amitha Ramesh. Resources: Biju Thomas, Amitha Ramesh. Software: Gauri Jayachandran, Amitha Ramesh, Mamatha Shetty. Supervision: Biju Thomas, Amitha Ramesh, Smitha Shetty, Mamatha Shetty. Validation: Biju Thomas, Sruthi Vijayan. Visualization: Gauri Jayachandran, Biju Thomas. Writing—original draft: Gauri Jayachandran, Smitha Shetty, Mamatha Shetty. Writing—review & editing: Gauri Jayachandran, Biju Thomas, Karthika Ganesh.
REFERENCES1. Hajishengallis G. Interconnection of periodontal disease and comorbidities: evidence, mechanisms, and implications. Periodontol 2000 2022;89:9-18.
3. Grossi SG, Genco RJ, Machtei EE, Ho AW, Koch G, Dunford R, et al. Assessment of risk for periodontal disease. II. Risk indicators for alveolar bone loss. J Periodontol 1995;66:23-9.
4. Haffajee AD, Socransky SS. Relationship of cigarette smoking to attachment level profiles. J Clin Periodontol 2001;28:283-95.
5. Nelson RG, Shlossman M, Budding LM, Pettitt DJ, Saad MF, Genco RJ, et al. Periodontal disease and NIDDM in Pima Indians. Diabetes Care 1990;13:836-40.
6. Suresh S, Mahendra J. Multifactorial relationship of obesity and periodontal disease. J Clin Diagn Res 2014;8:ZE01-3.
7. Jepsen S, Suvan J, Deschner J. The association of periodontal diseases with metabolic syndrome and obesity. Periodontol 2000 2020;83:125-53.
8. Hilgert JB, Hugo FN, Bandeira DR, Bozzetti MC. Stress, cortisol, and periodontitis in a population aged 50 years and over. J Dent Res 2006;85:324-8.
9. Shaddox LM, Morford LA, Nibali L. Periodontal health and disease: the contribution of genetics. Periodontol 2000 2021;85:161-81.
10. Wu L, Zhang SQ, Zhao L, Ren ZH, Hu CY. Global, regional, and national burden of periodontitis from 1990 to 2019: results from the global burden of disease study 2019. J Periodontol 2022;93:1445-54.
11. Janakiram C, Mehta A, Venkitachalam R. Prevalence of periodontal disease among adults in India: a systematic review and meta-analysis. J Oral Biol Craniofac Res 2020;10:800-6.
13. Irwin MR. Sleep and inflammation: partners in sickness and in health. Nat Rev Immunol 2019;19:702-15.
14. Dowd JB, Goldman N, Weinstein M. Sleep duration, sleep quality, and biomarkers of inflammation in a Taiwanese population. Ann Epidemiol 2011;21:799-806.
15. Maggio M, Colizzi E, Fisichella A, Valenti G, Ceresini G, Dall’Aglio E, et al. Stress hormones, sleep deprivation and cognition in older adults. Maturitas 2013;76:22-44.
16. Suri JC, Sen MK, Adhikari T. Epidemiology of sleep disorders in the adult population of Delhi: a questionnaire based study. Indian J Sleep Med 2008;3:128-37.
17. Grover V, Malhotra R, Kaur H. Exploring association between sleep deprivation and chronic periodontitis: a pilot study. J Indian Soc Periodontol 2015;19:304-7.
18. Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodontol 2018;89(Suppl 1):S159-72.
19. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193-213.
20. Kwon T, Lamster IB, Levin L. Current concepts in the management of periodontitis. Int Dent J 2021;71:462-76.
21. Page RC, Kornman KS. The pathogenesis of human periodontitis: an introduction. Periodontol 2000 1997;14:9-11.
22. Cochran DL. Inflammation and bone loss in periodontal disease. J Periodontol 2008;79(8 Suppl):1569-76.
23. Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry 2016;80:40-52.
24. Lorton D, Lubahn CL, Estus C, Millar BA, Carter JL, Wood CA, et al. Bidirectional communication between the brain and the immune system: implications for physiological sleep and disorders with disrupted sleep. Neuroimmunomodulation 2006;13:357-74.
25. Milrad SF, Hall DL, Jutagir DR, Lattie EG, Ironson GH, Wohlgemuth W, et al. Poor sleep quality is associated with greater circulating proinflammatory cytokines and severity and frequency of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) symptoms in women. J Neuroimmunol 2017;303:43-50.
26. Manzar MD, Moiz JA, Zannat W, Spence DW, Pandi-Perumal SR, Ba-Hammam AS, et al. Validity of the Pittsburgh Sleep Quality Index in Indian university students. Oman Med J 2015;30:193-202.
27. Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res 2002;53:737-40.
28. Sitasuwan T, Bussaratid S, Ruttanaumpawan P, Chotinaiwattarakul W. Reliability and validity of the Thai version of the Pittsburgh Sleep Quality Index. J Med Assoc Thai 2014;97(Suppl 3):S57-67.
29. Alqaderi H, Goodson JM, Agaku I. Association between sleep and severe periodontitis in a nationally representative adult US population. J Periodontol 2020;91:767-74.
30. Han DH, Kim MS, Kim S, Yoo JW, Shen JJ. Sleep time and duration are associated with periodontitis in a representative sample of Koreans. J Periodontol 2022;93:210-9.
31. Alhassani AA, Al-Zahrani MS. Is inadequate sleep a potential risk factor for periodontitis? PLoS One 2020;15:e0234487.
32. Romandini M, Gioco G, Perfetti G, Deli G, Staderini E, Laforì A. The association between periodontitis and sleep duration. J Clin Periodontol 2017;44:490-501.
Fig. 1. Mean sleep quality score according to stage and grade of periodontitis. Stage IV (p = 0.010) and Grade B (p = 0.004) subjects showed the highest mean in terms of sleep quality 
Fig. 2. Mean sleep duration score according to stage and grade of periodontitis. The highest mean of sleep duration was seen in patients with Stage IV (p < 0.001) and Grade B (p = 0.019) periodontitis. 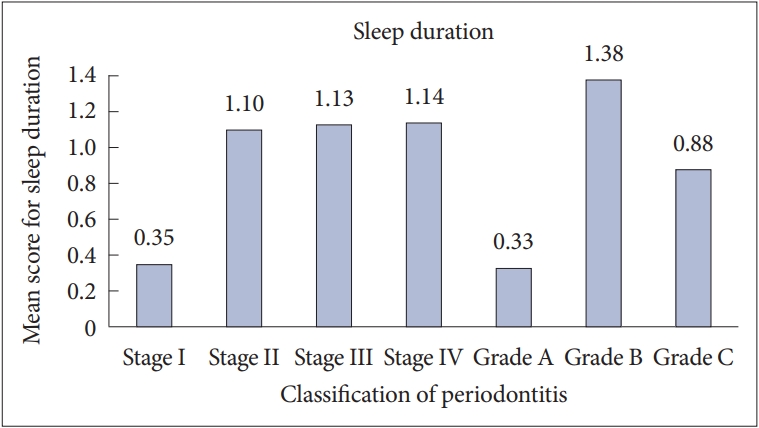
Table 1.Demographic characteristics of the patient’s sex and age who were included in this study Table 2.PD and CAL according to stage and grade of periodontitis
Table 3.Various components of the PSQI score according to stage and grade of periodontitis
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||