INTRODUCTION
Exploding head syndrome (EHS) is a rare parasomnia occurring either at the wake-sleep transition or upon waking during the night. It is characterized by typically painless loud bang or sense of explosion, sometimes less alarming sound in the head [1,2]. It might be accompanied by Jerky movements, a visual image such as flames, or explosive lights. Significant pain should not be associated with these sensory symptoms. Here I present a patient with EHS and obstructive sleep apnea (OSA) who had EHS symptom soon after a breathing event. To my knowledge, close temporal association EHS and sleep-breathing event with polysomnography have not been previously reported. This study followed the principles of the Declaration of Helsinki. It was approved by Inje University Busan Paik Hospital Institutional Review Board (BPIRB#: 2022-03-037). The requirement of informed consent was waived by the institutional review board.
CASE REPORT
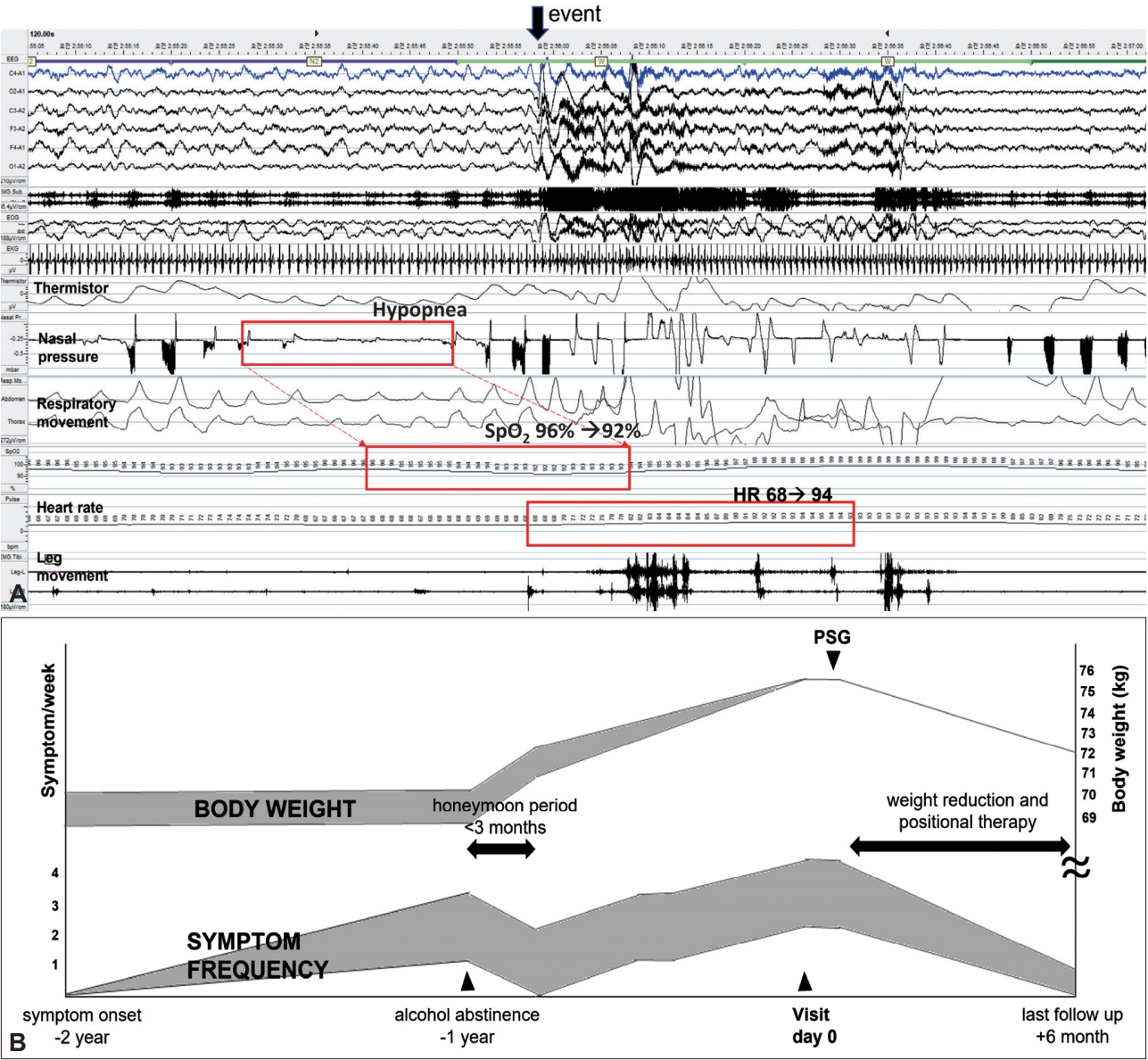
A 67-year-old man reported symptoms of a flash of visual lightning accompanying a small noise in his head during sleep for two years. It occurred in the middle of the night during sleep and lasted a few seconds. The patient was initially terribly frightened and embarrassed. He had difficulty falling asleep again. However, the frightening had gradually subsided over two years. Interestingly, the frequency increased when the patient consumed alcoholic beverages. Thus, the patient stopped drinking a year ago and the frequency decreased to once a week. However, these symptoms increased again after 3 months. It had increased to 2ŌĆō4 times a week (Fig. 1B). He had no headache, nausea, or vomiting, although the patient sometimes experienced jerky movement of his body. He had no history of migraine. He was taking a medicine for hypertension and hypothyroidism. Neurological examination, laboratories work up, brain MRI, and electroencephalography (EEG) were unremarkable. The patient was overweight (168 cm and 75 kg, body mass index 26.5 kg/m2). He snored loudly with frequent apnea. His insomnia severity index score was 19 (15ŌĆō21, moderate insomnia). His Epworth sleepiness scale score was 9 (0ŌĆō10, normal range of sleepiness). Polysomnography using extended 10ŌĆō20 EEG montages was done. Apnea-hypopnea index (AHI) was 67.6/h (supine AHI 80.1/h, lateral AHI 16.4/h). Minimal oxygen saturation was 77% and oxygen saturation below 90% time was 13.4/h (3.7%). Respiratory-related arousal index was 19.4/h. Spontaneous arousal index was 2.4/h and total arousal index was 24.0/h. Periodic limb movement index was 24.0/h. There was no EEG abnormality or rapid-eye movement-atonia dissociation. One episode was recorded at 2:50 AM when the patient experienced a typical flash of visual lightning in his head just after a hypopnea event. He woke up for 1 minute and slept again (Fig. 1A). He could recall the episode. The patient was diagnosed with EHS and positional OSA (supine AHI/lateral AHI > 2). I reassured the patient and recommended positive airway pressure (PAP) therapy considering the possible association between OSA and EHS. However, the patient refused PAP. Thus, positional therapy and weight reduction were recommended as alternatives. Since then, the patient followed positional therapy and lost his weight for about 3 kg. The frequency of symptoms has decreased to less than once a week at the last follow-up at 6 months (Fig. 1B). After a two-year loss to follow-up, I called the patient and interviewed him. The patient reported that the symptom persisted once every 1ŌĆō2 weeks after having positional therapy for one year. Although I could not check the adherence of auto-adjusting PAP or residual apnea downloaded from a machine, the patient said his symptom had almost disappeared for more than six months after an auto-adjusting PAP therapy at another hospital.
DISCUSSION
Current diagnostic criteria of EHS by the International Classification of Sleep Disorders, the third edition, do not mention the need to exclude a disorder not better explained by another sleep disorder such as OSA [1]. Thus, both EHS and OSA diagnoses can be made in this case. As visual symptoms were predominant in this case, sleep-related hallucinations should be differentiated. Sleep-related hallucinations might be accompanied by noise or flash of light. They occur frequently during the sleep onset and the rapid eye movement (REM) period of sleep-wake transition. However, visual hallucinations following a sudden awakening are usually complex with visual imagery lasting for a few minutes [1,3].
EHS is regarded as a sensory variant of sleep. It starts to occur during sleep-wake transition. Its pathologic mechanism is largely unknown [1]. Although OSA is known to cause disorders of arousals from non-rapid eye movement (NREM) sleep such as confusional arousals, sleepwalking, and sleep terrors [1], whether the prevalence of overall parasomnia symptoms is increased in patients with OSA is controversial [4,5]. Some studies suggest that the prevalence of sleepwalking is higher in patients with OSA in a dose-response manner [5]. Severe OSA can mimic REM sleep behavior [6]. Only limited cases or case series have reported the association between EHS and OSA with its symptom reversal after oral appliance or positional therapy [7,8]. However, the close temporal relationship between sleep-disordered event and EHS symptoms has not been reported yet.
The remaining question is whether it represents a coincidence between a rare parasomnia EHS and relatively common OSA, or whether OSA triggers EHS like the suggested mechanisms of hypoxemia and arousals between OSA and NREM parasomnia. As the patient had frequent breathing events during sleep, respiratory events and EHS symptoms might have occurred by chance. I suggest that OSA may trigger EHS in this case with the following reasons: 1) the close temporal relationship between a breathing event and symptom, 2) the positive effect of alcohol abstinence on symptoms and its possible reversal with weight gain, 3) the symptom reduction with positional therapy and weight loss, and 4) almost complete resolution of sleep with auto-adjusting PAP therapy. Alcohol consumption is associated with a higher risk of sleep apnea. It increases the risk of prolonged apnea events with OSA [9,10].
This report is based on my observation of the effect on EHS of alternative treatment of OSA during a limited follow-up period 6 months and my phone interview about the patientŌĆÖs symptom after auto-adjusting PAP therapy at another hospital. This report highlights that EHS might be associated with OSA. The causal link between EHS and OSA needs a further study.