Turkish Adaptation and Validation of the Adolescent Sleep-Wake Scale
Article information
Abstract
Background and Objective
The aim of our study was to evaluate the psychometric properties of the ASWS in a Turkish adolescent sample.
Methods
Two hundred and two Turkish high school students participated in our study. We used exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) for factor structure. McDonald’s ω and Cronbach’s α values were utilized for reliability analyses. We examined convergent validity by calculating correlations between the ASWS and sleep parameters and perceived stress scale scores.
Results
A 3-factor structure was detected, explaining 66.20% of the total variance with an eigenvalue above 1 in EFA. The 3-factor structure was confirmed with good fit indices in CFA. The scale demonstrated solid internal consistency (α = 0.844, ω = 0.832). We found a significant negative correlation between the ASWS and perceived stress, sleep latency, wakefulness after sleep onset, and ability to sleep after wakefulness at night.
Conclusions
The Turkish ASWS was found to be a valid and reliable instrument.
INTRODUCTION
Sleep quality emerges as an important indicator of well-being during adolescence. The prevalence of sleep problems in children and adolescents has been recognized as a major public health concern [1,2]. Adolescents are vulnerable to sleep disorders due to the interaction between significant biological, psychological, and sociocultural changes [3]. Sleep disorders in adolescents manifest in various ways, including inconsistent and delayed sleep patterns, decreased sleep duration, excessive daytime sleepiness, and insomnia [4-7]. Adolescents with medical conditions have even worse sleep problems [8,9].
The sleep-wake cycle in adolescents is influenced by circadian rhythms, delayed sleep phase, preference for evening chronotype, and hormonal changes [10,11]. Sleep-wake schedules set by schools may not be compatible with biological circadian and homeostatic processes that regulate adolescents’ sleep patterns [11,12]. Adolescents often experience a delayed circadian phase on weekends and holidays, resulting in late-night schedules and later waking times [13]. This process is exacerbated by the natural shift in circadian rhythms during adolescence and can lead to delayed sleep phase syndrome [14]. All these changes may contribute to sleep deprivation and poor sleep quality among adolescents [15].
Sleep impacts cognition, academic achievements, and daily activities [8,16]. Thus, it is crucial to investigate sleep quality throughout adolescence [17]. Some objective methods exist for assessing sleep-related parameters. The most essential objective methods are polysomnography and wrist actigraphy, which require a device, equipment, and a long time. However, many psychometric self-reported sleep instruments can be used in practice [18]. Since objective testing devices are unavailable in every clinic and their costs are high, self-reported sleep instruments remain the most practical method for evaluating insomnia in children and adults. The Adolescent Sleep-Wake Scale (ASWS) is a valuable tool for gathering information on sleep behavior and quality in adolescents. It is a multi-dimensional self-reported measure that provides a comprehensive assessment of sleep [19]. The ASWS was developed to assess adolescent sleep quality and difficulties. It supplies 3 subscale scores and an overall sleep quality score, with higher scores showing better success in each dimension and sleep quality. The ASWS is based on the ASWS-10, a 10-item measure developed by Essner et al. [20], which comprises 3 factors: falling asleep and staying asleep, waking up and functioning, and daytime sleepiness. The aim of our study was to evaluate the psychometric properties of the ASWS in a Turkish adolescent sample. These study findings contribute to improving sleep research and clinical practice in Turkey.
METHODS
Participants and Study Design
We randomly selected participants from high school students in Erzurum for the study. The study included 202 high school students (44.1% female and 55.9% male). The participants’ ages ranged from 14 to 18 years. More than half of the participants had a medium family income level. A very small proportion (2.5%) of the participants had a history of sleep disorders. Of the participants, 13.9% had a family history of sleep disorders, 11.4% had any disease, and 13.4% were using any medication. Table 1 shows the sociodemographic and clinical variable details of the study sample. The participants completed a sociodemographic and sleep data form and the Turkish version of the ASWS and the Perceived Stress Scale (PSS). All patients and participants read and signed an informed consent form before completing the sociodemographic and sleep data form and the psychological tools. The study was approved by the Ethical Committee at the Faculty of Medicine at Ataturk University (approval date and decision number: June 7, 2023; 5/78). The study was conducted between September 1, 2023, and October 15, 2023.
Adaptation and ASWS Pilot Test
The ASWS is a 10-item measure of subjective sleep quality for adolescents [21]. It has a 6-point Likert scale structure. Each item asks about sleep characteristics in the past month, and the answers are scores on a range from 1 (never) to 6 (always). After the pilot test, we redesigned the item responses to a scale of 1 for never, 2 for once in a while, 3 for sometimes, 4 for quite often, and 5 for always. The total score was obtained by summing the scores for all items. Higher scores indicated better sleep quality. Essner developed the 10-item ASWS [20]. The scale has a 3-factor structure: going to bed (items 1, 2, and 3), falling asleep-reinitiating sleep (items 4, 5, 6, 7, and 8), and returning to wakefulness (items 9, 10) [20,21]. Cronbach’s α for these subscales were calculated to be 0.71, 0.84, and 0.87, respectively [20].
We obtained permission from Monique K. LeBourgeois, the original developer of the ASWS, to translate and adapt it into Turkish. The language validity of this scale was determined by the back-translation method. Three native Turkish speakers separately translated the scale from English to Turkish. The research team thoroughly analyzed the translations and carefully selected the Turkish terms that best represented each English item, forming the Turkish scale. A native English speaker translated the Turkish version of the scale back into English, and then we compared the original scale to this translation to ensure compatibility. Ultimately, the study team deliberated on the scale elements and determined the final version.
We applied the final version of the scale as a pilot test to a group of 10 people similar to the study sample and received their explicit opinions about the scale items and options (pilot test participants were not included in the study). In open interviews with the pilot test participants regarding the response options of the scale, we removed the answer ‘‘frequently, if not always,’’ considering that it had a very similar meaning “quite often” in Turkish. We redesigned item responses of the scale as 1 for never, 2 for once in a while, 3 for sometimes, 4 for quite often, and 5 for always. Finally, we used the Davis method to determine the content validity of the scale. We sent the final version of the ASWS to 10 sleep medicine experts via e-mail. Each expert rated each item using a 4-point scale (1 = not clear, 2 = need some revision, 3 = clear but need minor revision, 4 = very clear). All items received a Content Validity Index score above 0.83. Therefore, no item required revision or was excluded based on content validity.
Other Instruments
Sociodemographic and sleep data form
We used a questionnaire to obtain demographic and sleep data. The first part asked about age, sex, educational status, chronic illness, history of sleep disorders, and parental history of psychiatric illnesses. In the second part, we asked the following 3 questions: 1) Sleep latency (SL; in minutes)—How long did it usually take you to fall asleep in the last month?; 2) Wakefulness after sleep onset (WASO; in numbers)—How many times did you awake at night after falling asleep in the last month?; and 3) Ability to fall asleep after wakefulness during the night (AAWASO; in minutes)—In the last month, how many minutes did it take for you to fall back asleep after waking up at night?
Perceived Stress Scale
The PSS is a 14-item scale used to assess self-perceived stress. It consists of 14 items and measures how stressful some situations in a person’s life are perceived [22,23]. The participants evaluated each item on a 5-point Likert-type scale ranging from 0 for never to 4 for very often. The total scores range from 0 to 56, with higher scores indicating higher levels of perceived stress. Cronbach’s α was α = 0.83 in our study.
Study sample size
The total number of participants was 202. The calculated minimum sample size was 10 participants for each scale item [24]. Since ASWS has 10 items, at least 100 participants were required. In addition, regardless of the number of items on a scale, at least 200–300 participants are recommended for factor analysis [25,26]. The sample size of the present study was sufficient according to the ideal ratio of respondents to items (10:1) and the assumption of 200–300 participants.
Statistical Analysis
We used SPSS 23.0 (IBM Corp., Armonk, NY, USA) and jamovi 2.3.18 (The jamovi project; www.jamovi.org) for the analyses. Descriptive statistics identified means, standard deviations, and frequencies. The skewness kurtosis value was used to determine the normality of the data. Hair et al. [27] and Bryne [28] argued that data is considered to be normal if skewness is between -2 to +2 and kurtosis is between -7 to +7. We assessed the factor structure of ASWS by both exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). We calculated Cronbach’s α and McDonald’s ω for reliability analyses. The correlations between the ASWS and SL, WASO, AAWASO, and PSS scores were analyzed using Pearson’s or Spearman’s correlation coefficient to determine the convergent validity of the ASWS. We accepted the following values for fit index values: χ2/df (chi-squared/degree of freedom) less than 5.0, comparative fit index (CFI) greater than 0.90, Tucker-Lewis index (TLI) greater than 0.90, and a standardized root-mean square residual (SRMR) close to or below 0.08 [29-31]. Reliability values above 0.70 and items with a factor load > 0.30 were interpreted as meaningful and were accepted [32,33]. A p-value of less than 0.05 was considered statistically significant.
RESULTS
Descriptive Statistics and ASWS Factor Analysis
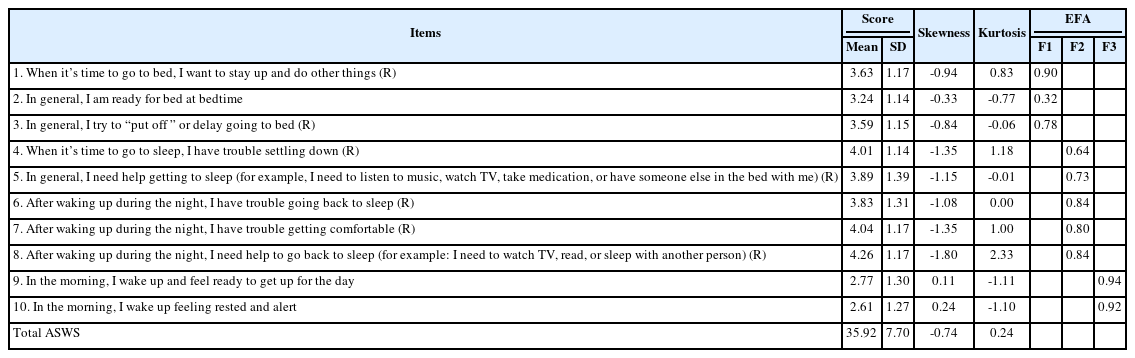
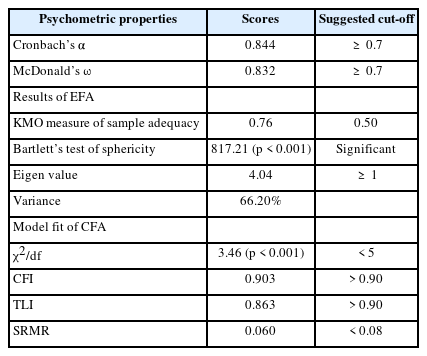
Table 2 presents the item-level properties. Skewness (ranging between -1.80 and 0.24) and kurtosis values (ranging between -1.11 and 2.33) suggested normality of the item-level data. We performed EFA for factor analysis. The Kaiser-Meyer-Olkin value (0.76), Bartlett’s test of sphericity (χ2 = 817.21, p < 0.001) suggested the suitability of the data for EFA (Table 3). The EFA results (Table 3) indicated that each of the 3 factors had an eigenvalue above 1 (4.04). Factor analysis with oblimin rotation suggested that the 3 factors had an eigenvalue of 4.04 and explained 66.20% of the scale variance. Items 1, 2, and 3 clustered in Factor 1. Items 4, 5, 6, 7, and 8 clustered in Factor 2, and 9 and 10 clustered in Factor 3. The factor loading of EFA items ranged between 0.32 and 0.94, above the recommended cut-off. Table 2 shows the factor loadings of the EFA items. The CFA analysis showed that the 3-factor structure had the following models of fit: χ2 = 111, df = 32, p < 0.001, χ2/df = 3.46, CFI = 0.903, TLI = 0.863, and SRMR = 0.060. These values suggest a good fit. Table 3 shows the details of these analyses.
Reliability Analysis
The scale had sound internal consistency (α = 0.844, ω = 0.832). Cronbach’s α and McDonald’s ω did not increase when removing items.
Convergent Validity (Association of the ASWS with SL, WASO, AAWASO, and PSS Scores)
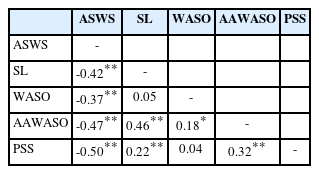
We used Pearson’s correlation with other tools to analyze convergent validity. We determined significant negative correlations between ASWS total scores (greater scores indicated better sleep) and SL (r = -0.42, p < 0.01), WASO (r = -0.37, p < 0.01), AAWASO (r = -0.47, p < 0.01), and PSS (r = -0.50, p < 0.01) scores in our study. No significant correlation was detected between ASWS scores and age (Table 4).
DISCUSSION
In the current study, we adapted the original version of the ASWS to Turkish and evaluated the psychometric properties of the adapted version. The present study was the first to validate the performance of the Turkish ASWS. The main findings of our research were that the Turkish ASWS had a 3-factor structure (going to bed, falling asleep-reinitiating sleep, and returning to wakefulness) with good fit indices. It had good internal consistency (Cronbach’s α = 0.844 and McDonald’s ω = 0.832). We found a significant negative correlation between ASWS scores (greater scores indicated better sleep) and sleep latency, number of awakenings during the night, ability to go back to sleep after waking up at night, and perceived stress.
ASWS is the most widely used scale of sleep quality designed for adolescents [19,34]. The ASWS long form contains 28 items. ASWS 10 was prepared from the long form by Essner et al. [20]. The 10-item ASWS can be more practically and easily applied in clinical use. Therefore, we aimed to adapt the ASWS 10-item form into Turkish and examine its psychometric properties. Essner et al. [20] showed that ASWS 10 items had good fit indices in a 3-factor structure. They organized these 3 factors as items 1, 2, 3 (going to bed), items 4, 5, 6, 7, and 8 (falling asleep and reinitiating sleep), and items 9 and 10 (returning to wakefulness). In addition to these factors, the ASWS 28-item form included 2 more factors: falling asleep and maintaining sleep. These 2 factors are not included in ASWS 10. However, information on these issues was obtained by asking the participants 2 additional questions regarding these factors: sleep latency and maintaining sleep. Like Essner et al. [20], we determined ASWS to have a 3-factor structure. We named these 3 factors “going to bed,” “falling asleep-reinitiating sleep,” and “returning to wakefulness.” In our study, the same items were included in the same group as in the original scale. In our research, we also examined the factor structure using EFA. In EFA, we detected a 3-factor structure explaining 66.20% of the total variance above an eigenvalue of 1.
Essner et al. [20] found a total Cronbach’s α of 0.81 for the ASWS scale. We found it to be 0.84, and the Turkish ASWS showed strong internal consistency. Since higher ASWS scores represent better sleep, it was expected that ASWS scores would show a significant negative correlation with factors such as sleep latency and sleep disturbance. In this regard, previous studies found that the ASWS-28 and ASWS-10 scales negatively correlated with sleep latency, sleep disturbance, and daytime dysfunction [20,21,34]. In our research, we found significant negative correlations between ASWS and sleep latency, the number of awakenings during the night, the ability to go back to sleep after waking up at night, and perceived stress.
This study had several limitations. First, the participants were from a single city. Therefore, our results cannot be generalized to the entire Turkish adolescent population. Second, we did not conduct a clinical interview and evaluated the participants using only scales. Third, we could not determine the cut-off value for the ASWS since our study lacked clinical interviews. Fourth, we could not perform a retest-test analysis. Fifth, we did not assess the association between ASWS scores and objective measures of sleep (e.g., polysomnography). Despite these shortcomings, this was the first study in which ASWS was adapted into Turkish. Future studies should include studies with larger samples and clinical populations. The researchers should also add objective measures of sleep to ASWS validation studies.
Notes
Availability of Data and Material
The datasets are available from the corresponding author upon reasonable request.
Authors’ Contribution
Conceptualization: Omer Faruk Uygur, Abdullah Bozkurt. Data curation: Abdullah Bozkurt, Omer Faruk Uygur. Formal analysis: Omer Faruk Uygur. Methodology: Abdullah Bozkurt. Resources: Abdullah Bozkurt, Esen Yildirim Demirdogen. Software: Omer Faruk Uygur, Abdullah Bozkurt. Supervision: Abdullah Bozkurt, Omer Faruk Uygur. Validation: Abdullah Bozkurt, Esen Yildirim Demirdogen. Visualization: Abdullah Bozkurt, Esen Yildirim Demirdogen. Writing—original draft: Abdullah Bozkurt, Esen Yildirim Demirdogen. Writing—review & editing: Abdullah Bozkurt, Omer Faruk Uygur.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Funding Statement
None
Acknowledgements
We obtained permission from Monique K. LeBourgeois, the original developer of the ASWS, to translate and adapt it into Turkish.