Restless Legs Syndrome and Morningness-Eveningness in the Korean High-School Students
Article information
Abstract
Background and Objective
Restless legs syndrome (RLS) lowers the quality of sleep, and is characterized by symptoms that follow a circadian pattern. The aim of this study was to determine the relationship between RLS and morning-eveningness in Korean adolescents.
Methods
Of the 867 community-dwelling high school students, 590 subjects were included in this study. All participants completed self-report questionnaires, including demographic variables, particulars about menstruation, life style, sleep duration, RLS severity, Composite Scale, Epworth Sleepiness Scale, Insomnia Severity Scale, Patient Health Questionnaire-9 (PHQ-9), Pittsburgh sleep quality index and Berlin Questionnaire.
Results
Participants with RLS symptoms had a higher prevalence of depression, defined by a PHQ-9 score ≥ 10 (OR 3.03, CI 1.11–8.26) and eveningness in chronotype (odds ratio 1.95 confidence interval 1.15–6.43) when adjusted for depression, excessive daytime sleepiness, insomnia symptom and morningness-eveningness. However, RLS symptoms had no association with excessive daytime sleepiness and insomnia, when adjusted for clinical factors.
Conclusion
sIn Korean high school students, restless leg symptom may be preceded by depression and eveningness of chronotype. For healthy sleep lifestyle in the adolescents, an appropriate evaluation of RLS symptom as well as chronotype is recommended.
INTRODUCTION
Rapid physical growth, and development of physiological and behavioral maturity are associated with adolescence [1]. A cross-sectional study for Canadian high school students showed that up to 70% of students get less than the recommended amount of sleep for their age [2,3]. Sleep disorders may affect 25–50% of youth during infancy, childhood, and adolescence [4]. South Korean adolescents complain of severe sleep deprivation due to academic stress, which leads to the development of irregular sleep/wake pattern [5]. Due to schoolwork, students tend to stay awake late at night during weekdays, and wake up late on weekends to compensate for sleep debt during the week. An earlier study reported the evening chronotype on daytime and nighttime behaviors in adolescence [6]. The morningness-eveningness, such as morning/day activity (i.e., morningness) or evening/night activity (i.e., eveningness), is another indicator for circadian rhythm. During adolescence, the circadian pattern generally undergoes a change. This change, along with the early start of school activities, aggravates sleep deprivation in adolescents [5,7]. Disruption of the circadian pattern might also have an effect on emotional instability, decline in neurocognitive function, low social function, and decreased quality of life [8,9]. Particularly, it is documented that eveningness has an impact on depression in adolescents [6,10].
The neurological symptom associated with restless legs syndrome (RLS) is a pronounced urge to move the legs, typically accompanied with unpleasant sensations [11]. The prevalence of RLS is 5% to 10% in several large population-based studies in the US and Europe [12]. In the pediatric and adolescent populations, a prevalence of 2–2.6% has been reported [13,14]. RLS is a circadian disorder that mainly affects patients in the evening or at night [15]. The impact of RLS on sleep, particularly sleep-onset insomnia, contributes to the overall adverse impact on quality of life, often leading to serious psychosocial impairment [16]. In adolescents with irregular circadian pattern, restless leg symptoms could be influenced by their chronotype. However, very few studies have investigated the relationship between RLS and morningness-eveningness. Thus, the aim of this study was to investigate the relationship of RLS symptoms with morningness-eveningness in a community sample of Korean adolescents.
METHODS
Subjects and Procedures
This study was conducted between January 2015 to July 2015, by enrolling adolescents living in Anseong-si, Gyeonggi-do, Korea. Out of a total 867 students in the tenth grade of Anseong-si residents, we randomly selected 635 subjects (73.2%). Data were collected through self-report questionnaires, including demographic variables, sleep parameters, psychiatric assessment, and particulars about menstruation. The caffeine user was defined as a subject who regularly consumed coffee, cola, black tea or any other drinks containing caffeine, and smoker was defined as regularly smoking more than one cigarette a day. Informed consent was obtained from all subjects. Psychiatric and sleep assessments were performed as follows: the Composite Scale (CS) examined the morning-eveningness pattern, such as morning, intermediate or evening types; the Pittsburgh sleep quality index (PSQI) evaluated subjective sleep complaints; the Epworth Sleepiness Scale (ESS) assessed the daytime sleepiness; the Insomnia Severity Index (ISI) checked symptoms of sleep disturbance; the Patient Health Questionnaire-9 (PHQ) evaluated the mood symptoms; and the Berlin Questionnaire (BQ) was used to investigated snoring and sleep apnea. To assess RLS core symptoms, one question was presented as follows: “In the past year, did you have uncomfortable feelings in your legs while resting at night?” This question aimed to capture 3 out of 4 major clinical characteristics of RLS, namely uncomfortable feeling in the legs, which are worse at rest and at nighttime. Subjects were instructed to respond on a 5-point Likert scale (0 = never, 1 = less than once per month, 2 = 1–2 times per month, 3 = 1–2 times per week, 4 = equal to or more than 3 times per week). Subjects with a response of 4-point or more, were defined as having RLS symptoms. Finally, subjects having positive RLS symptoms in the questionnaire, were interviewed for confirmation of RLS. Psychiatrist with expertise in sleep disorders had face-to-face interviews with the subjects who were deemed eligible for the diagnostic phase. RLS was diagnosed based on the International RLS Study Group Rating Scale (IRLS) criteria. This study protocol had prior approval by the Institutional Review Board.
Measurements
The PSQI is composed of 19 items, covering seven components: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction [17]. The global score of PSQI ranges from 0 to 21. The ISI is a self-report questionnaire developed for measuring subjective insomnia severity of the patient [18]. The global score of ISI ranges from 0 to 21. In this study, insomnia (+) was defined as ISI score ≥ 10. The ESS is an item for measurement of general daytime sleepiness of the subject. The ESS comprises 8 questions that are rated on a 3-point Likert Scale. In this study excessive daytime sleepiness (+) was defined as an ESS score ≥ 10. The CS, which contains 13 items, was developed to measure three circadian rhythms, including morningness, intermediate, or eveningness of the chronotype [19]. The total score ranges from 12 to 55, where morningness-eveningness were defined as intermediate type with a score from 27 to 40, morningness type as 41 or more, and eveningness type as 26 or less. The PHQ-9 is a depression module that consists of 9 criteria upon which the diagnosis of DSM-IV major depressive disorders is based [20]. In this study, depression (+) was defined as PHQ-9 score ≥ 10. The BQ is an instrument validated for use in a western population to determine the presence of risk factors for obstructive sleep apnea [21]. We used 5 out of the 6 items of first category in the Korean version BQ, to evaluate snoring and obstructive sleep apnea of the subject [22].
Statistical Analysis
The Kolmogorov-Smirnov test for verifying normality of collected data was performed. Intergroup differences between two groups were assessed using chi-square test and independent t-test. Significant different variables between two groups were entered as independent variables, and single and multiple logistic regression analysis was done with RLS groups as dependent variable. The statistical significance criterion was defined to be p < 0.05 for two-tailed test. IBM SPSS Statistics for Windows, version 21.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis.
RESULTS
Comparison of Demographic Characteristics and Psychological Variables
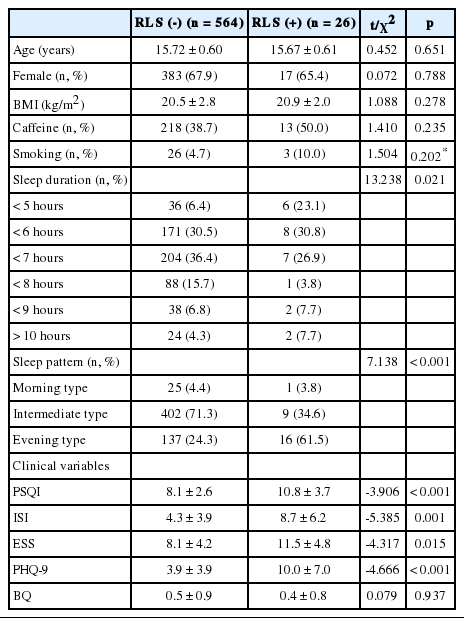
A total of 635 tenth grade participants completed the questionnaires. Of these, 590 students were eventually included as an appropriate sample; 45 subjects who did not answer all the questions thoroughly, were excluded. Based on presence of RLS, the subjects were classified into two groups. Of the 590 subjects participating in the screening phase, 48 subjects took part in the diagnostic phase. Among these 48 subjects, 26 subjects were categorized as the RLS group, and 564 subjects were classified as the non-RLS group. There were no significant differences in age, BMI, caffeine intake, and smoking, between the two groups. In the sleep parameters, the RLS group showed a shorter sleep duration (p = 0.021) and a higher evening type sleep/wake pattern (p = 0.028) compared to the non-RLS group. The RLS group was shown to suffer from poorer sleep quality with a higher PSQI score (p < 0.001), more severe insomnia symptoms based on the ISI score (p = 0.001), and more daytime sleepiness based on the ESS (p < 0.001), than the non-RLS group. Additionally, the RLS group showed more severe depressive symptoms based on the PHQ-9 (p < 0.001), relative to the non-RLS group (Table 1).
Clinical Data on Researched Students, Including Unadjusted and Adjusted Odds Ratio for RLS Symptom
Single and multiple logistic regression analysis were performed with RLS groups as dependent variable, and clinical variables as independent variables (Table 2). Participants with RLS symptoms had higher prevalence of depression defined as PHQ-9 score ≥ 10 [odds ratio (OR) 3.03, 95% confidence interval (CI) 1.11–8.26] and eveningness in chronotype (OR 1.95, 95% CI 1.15–6.43) when adjusted for depression, excessive daytime sleepiness, insomnia symptom and morningness-eveningness. However, RLS symptoms had no association with excessive daytime sleepiness and insomnia symptom when adjusted for clinical factors.
DISCUSSION
In this study, we investigated the relationship of RLS symptom with morningness-eveningness in Korean high school students. Among the participants who completed the questionnaires, 4.4% reported significant RLS symptoms. A large population-based study, comprising 2182 Hong Kong Chinese adolescents using the same questions for assessing RLS symptoms, reported a prevalence of 2.6% RLS [14]. This considerable difference might be due to a different scoring of diagnostic tool for RLS, our small sample size, and prevalence of female subjects. Previous studies were performed with the National Institutes of Health pediatric RLS diagnostic criteria, or the International RLS Study Group Rating Scale (IRLS), to evaluate RLS. Although the Hong Kong study used the questionnaire similar our study, their large sample size might have statistical power to study.
In patients having RLS symptoms, sleep disturbance is a very common problem, and in a clinical setting many patients with RLS visit the clinic complaining of sleep disturbance [23]. In the present study, there were significant differences in total sleep duration between the RLS and non-RLS groups. In past studies, subjects with RLS had difficulty falling asleep and difficulty maintaining asleep, which resulted in lower sleep efficiency and daytime sleepiness. Thus, they showed daytime dysfunction [16,24]. Higher proportions of the eveningness in the RLS group compared to the non-RLS group might be induced by symptoms of RLS causing greater difficulty in falling asleep [25]. In addition, the RLS group had prevalent depressive symptoms. These findings are consistent with those of previous studies which report depressive symptoms as being more common in adults with RLS, relative to the general population [26,27]. Previous studies also reported eveningness developed due to the insomnia symptom, which is usually caused by depression [28,29]. Although depression had higher odd ratios with RLS in our findings, RLS symptom also showed a mild association with eveningness. There are few studies directly associating RLS and chronotype. However, symptoms of RLS have a characteristic circadian pattern. Melatonin hormone, which exerts an inhibitory effect on central dopamine secretion, modulates the intensity of subjective complaints of RLS, and worsens RLS symptoms in the evening and during the night [30]. In the clinical study, rotating shift workers had significantly higher prevalence of RLS than workers with permanent morning work schedule [31]. Thus, the disturbance of circadian rhythms could affect the prevalence and intensity of RLS symptoms. More studies are required to evaluate the association of RLS with chronotype.
There are some limitations to this current study. Most importantly, this study had a cross-sectional design, which is unable to identify a causal relationship. Second, RLS was assessed by a self-report questionnaire, which is not a tool as validated as clinical interview with the National Institutes of Health pediatric RLS diagnostic criteria, or IRLS [32]. In addition, using RLS as a screening tool, there was a possibility of excluding RLS patients. Self-report of RLS could have a general tendency toward a negative, more exaggerated description of symptoms. Third, since this study was solely performed in the tenth grade in Anseong-Si, the results should be considered cautiously before applying these findings to other adolescents and clinical patients with RLS. Nevertheless, this study has evaluated the effect of RLS symptom on morningness-eveningness in tenth grade Korean students. In Korean adolescents, individuals with RLS symptom had more eveningness in chronotype, poorer sleep quality and depression, than those without RLS symptom. The RLS symptom might be risk factors for eveningness in sleep/wake pattern. Thus, an appropriate evaluation of RLS symptoms could help achieve a more effective treatment of eveningness, and enhance sleep quality and studying performance in adolescent students.
Acknowledgements
The authors wish to thank all those who helped to collect the data and those who kindly volunteered to participate in the study.
Notes
Conflicts of Interest
The author has no financial conflicts of interest.